Pandemic shows power of doctor's phone call to provide care
Federal government recently announced funding to expand online access to health care
It was intended as an interim measure to protect people during the pandemic, but now that doctors across Canada have embraced virtual care, some clinicians and patients would like to see it continue.
Earlier this week, Prime Minister Justin Trudeau announced more than $240 million in funding to expand the capacity for virtual health care by, among other things, creating digital platforms and apps and improving access to online mental health supports.
Moving some services online could ease the burden on the health care system when patients don't need to see their family physician, pediatrician or nurse practitioner in person.
Dr. Danielle Martin, a family physician with Women's College Hospital in Toronto, has been delivering virtual care as part of COVID-19 precautions. She says she's watched an "explosion" in virtual delivery of primary and specialty care across Canada and globally.
"Once you've got that relationship established [with a patient], a phone call can go a really long way in solving lots of problems," Martin said.

She gave the example of someone monitoring their blood pressure at home, emailing their readings to their doctor and then having a seven-minute phone call to renew a prescription for medications.
In the 1980s, Canada was considered a pioneer in the use of telemedicine to deliver health services to rural communities at a time other countries weren't thinking about it, Martin said.
Since then, broader uptake in Canada's publicly funded health care system has been slow, and private virtual health apps have taken off. But now, amid the pandemic, all provincial and territorial governments are covering appointments with family doctors by phone and video call — though they plan to stop paying for virtual visits this summer.
Before the pandemic, about four per cent of primary care visits in Canada were done virtually (phone, video, text or app). The most recent statistics show that has climbed to 60 per cent, according to Canada Health Infoway, a federally funded not-for-profit organization with a mandate to promote digital health solutions.
Less duplication of tests
At least one study has found that virtual health care has benefits.
Dr. Paul Wallace, a retired general practitioner with Digital Health London, conducted a randomized control trial of virtual medical consultations with nearly 3,000 British patients.
Wallace found that when patients, their family doctor and their specialist all met together online, fewer tests were ordered, cutting costs.

"The fact that the clinicians were sitting together and could actually make sure that that duplication didn't happen, could provide the information about previous tests, was actually one of the most powerful reasons why," Wallace said.
Patient satisfaction scores were also higher, he said, since patients were seen at the appointed time.
Wallace and other physicians acknowledge there will always be a need for in-person care, but with the technological advances made since that study in 2004, he estimates 50 to 70 per cent of primary care can be handled effectively by phone — maybe even more with secure video platforms that allow a clinician to assess something they might need to see, such as the way a patient's mole is changing, for instance.
Reduces stress
Since the COVID-19 pandemic began, Patricia Costa of Vaughan, Ont., has been using the video conferencing platform Zoom as well as the phone to check in regularly with her specialist.
"She's engaged in the communication the way she's always been," Costa said. "If anything, there's greater benefits with having less stress … breaking down those barriers of driving, parking, frequency of appointments."
Costa said the virtual appointments lighten her scheduling pressures while caring for her children, aged nine and 12.
She hopes virtual care will be able to continue after the pandemic ends.
Martin hopes so, too.
"We're not in a situation where we can sort of say, 'Well, we're just going to go back to the way that it was before,' because I think patients have had a taste of this convenience, and I don't think that they want to go back," Martin said.
But there are other considerations if virtual care is to ramp up, including the ability to provide translation services for those who need them, and to accommodate those who have disabilities or other barriers to using technology.
The Canadian Medical Association's virtual care task force recommended in February that governments make virtual care a priority, with common safety and quality standards across the country.
"I think this is an instance where we need to hang on to one of the small goods that came out of the pandemic and that is the ability of our health care system to change rapidly on a dime to accommodate the changes that needed to be made," said Dr. Gigi Osler, who co-chaired the task force.
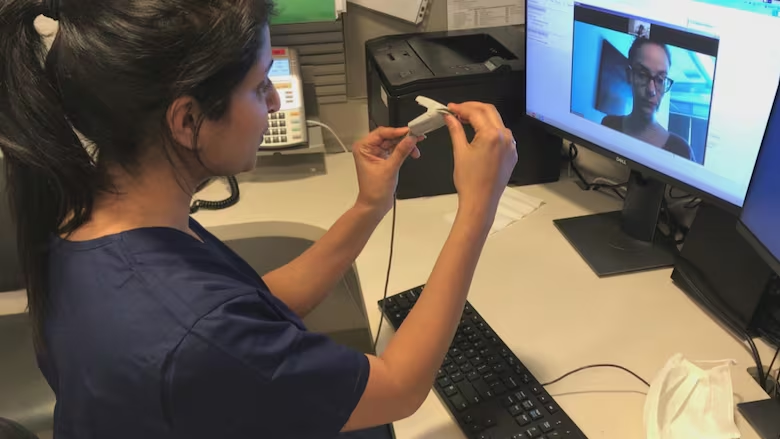
WATCH | Virtual care takes off during COVID-19 crisis
With files from CBC's Vik Adhopia and Melanie Glanz

