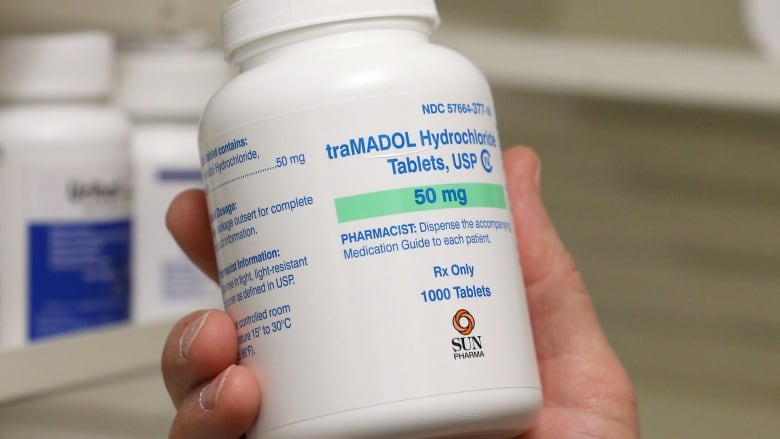
'There really is no safe opioid': Study finds tramadol isn't a less addictive painkiller
Prescriptions for post-surgery pain are on the rise, but they shouldn't be, researchers say
There is no such thing as a safe opioid.
That's the message of a study published in The BMJ this week.
American researchers found that tramadol, an increasingly prescribed post-surgery painkiller that was thought to be less addictive than other opioids, is actually every bit as dangerous.
Along with his team, lead author Cornelius Thiels, chief resident in general surgery at the Mayo Clinic in Rochester, Minn., combed through prescription records of more than 444,000 patients across the U.S. who had surgeries between 2009 and 2018.
The team found that at least seven per cent of patients refilled their opioid prescription three to six months after surgery — and the most commonly prescribed opioid was tramadol.
"What we know now is there really is no safe opioid, and tramadol is not a safe alternative," Thiels said. "Tramadol essentially has a similar risk of long-term dependence or long-term opioid use compared to other opIoids."

The BMJ study comes on the heels of a scientific review of tramadol conducted by Health Canada. The agency noticed a risk of serious breathing problems in some patients who metabolize tramadol quickly, and is now considering tightening regulations for the drug.
"Evidence showed that high doses of tramadol have the same risks of dependency and problematic use as stronger opioids, such as morphine," Health Canada spokesperson Maryse Durette said in an email.
The opioid epidemic in North America took off about a decade ago with massive increases in prescriptions of narcotic painkillers such as OxyContin, fentanyl, codeine and hydrocodone.
The problem was made even worse by an illicit fentanyl crisis that Health Canada says is behind the majority of the country's opioid-related overdose deaths.
Opioids block pain, and can also induce euphoria. Over time, the body builds up a tolerance to the initial rush, so that ever higher doses are needed to produce the same effect. Opioids also depress breathing, causing sleepiness at low doses. During an overdose, breathing can slow down so much that it finally stops, causing death.
Tramadol was first licensed internationally in the 1970s. In Canada, it is sold under brand names such as Ultram and Durela.
The drug is suspected to have contributed to 18 reported deaths across the country between 2006 and 2017, according to federally compiled statistics.
New definition of a successful surgery
Health Canada says consumption of tramadol has been increasing over the past few years.
Thiels said he's noticed the same trend at his hospital in the U.S., but it's time to "reverse course" and cut back on its use.
The goal is to reduce how many people become dependent on opioids after surgery — a problem Thiels says should be treated as seriously as other surgical complications, such as infection.
If someone stays on opioids long-term after surgery, it's not a successful surgery, he said.
The risk starts to increase after five to seven days of taking the drugs.

Thiels advocates not prescribing any opioids after surgery, when possible. Instead, he recommends alternatives like non-steroidal anti-inflammatories (NSAIDs), such as ibuprofen, to control pain.
The focus on trying to avoid using opioids in the health-care system should have started years ago, Thiels said, but better late than never.
"We are having a dramatic kind of success in reversing or preventing new addiction, but I think there's a lot more work to be done for those who are already … dependent on opioids."
Taper slowly
Dr. David Juurlink, head of clinical pharmacology at the University of Toronto, said the BMJ study shows that some doctors are "less aggressive" about getting patients off tramadol because they don't perceive it to be "as hazardous as it sometimes can be."
He explained that our bodies convert tramadol into an opioid. But individuals metabolize it at different rates, and on average, seven in 100 people don't get any pain-relieving effect at all, he said.
He recalled one case where a man saw a surgeon who wanted to prescribe him Percocet, which contains the opioid oxycodone, for a shoulder problem.
"The patient said, 'I'd rather not go on opioids,' and the surgeon said, 'Well, here's some tramadol,' apparently not realizing that tramadol is converted to an opioid," said Juurlink, who is also a scientist at the Institute for Clinical Evaluative Sciences in Toronto.
More than a year later, Juurlink said the man faced "crippling insomnia" when he tried to cut back on the drug on his own.
"We just tapered him off very, very slowly and his life is much better now. But I don't know how many times that particular anecdote has played itself out in Canada over the last 10 or 15 years."
Proceed with caution
That's why Juurlink has called on Health Canada to act immediately to reclassify tramadol under the Narcotic Control Regulations.
"I'm not saying that tramadol should come off the market. I'm saying that it is not a drug that deserves this preferential classification that Health Canada accorded it more than a decade ago," he said.
By reclassifying tramadol from a prescription drug to a narcotic, doctors would no longer be able to phone in prescription renewals for it without first seeing the patient to discuss if he or she still needs it.
Juurlink also said tramadol's marketing and federal classification makes a psychological difference to prescribers. The misleading message they receive today is that tramadol is "somehow less encumbered by risks of addiction and dependence," he said.
If and when Health Canada's proposed regulations that would add tramadol to its Schedule 1 list of drugs with the highest risk of dependence are enacted, they would go into effect a year later.
Health Canada's Maryse Durette said the proposed regulations would help:
- Reduce the health risks associated with the improper use of tramadol.
- Strengthen the surveillance of tramadol prescribing practices.
- Provide Canadian law enforcement agencies with the authority to take action against unauthorized activities involving tramadol.
"The proposed regulatory changes will not take medication away from those who need it and will not affect the way that patients currently access this prescription medication," she said.
The proposal is open for public comments until June 18.