Do I have COVID-19, the flu or a cold?
What to do if you have symptoms and are worried you've been exposed to COVID-19
Public health officials believe the rate of COVID-19 cases in Canada is going to get worse before things start to get better. If you feel sick, when should you get tested?
Here are some basic facts about the virus, its symptoms, prevention, and what to do if you believe you are infected. There is also some information about asymptomatic carriers, who may be infecting more people than anyone initially realized.
What are the symptoms?
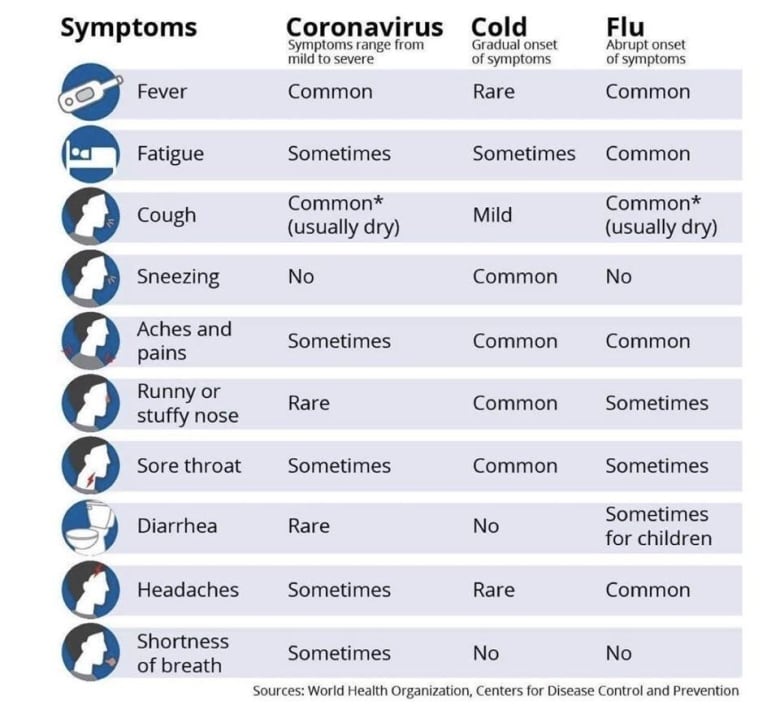
Unfortunately, the initial symptoms of COVID-19 are very similar to the seasonal flu and even the common cold, so you may not know whether you are infected with COVID-19.
The symptoms can include:
- Fever.
- Cough.
- Difficulty breathing.
- Digestive symptoms such as diarrhea.
- Pneumonia in both lungs (which would be seen on a chest X-ray).
A study of 10 children in China released on March 13 found children experienced milder and slightly different symptoms. None had a fever over 39 C, none had the muscle aches and headaches that adults often do with this disease, and none had pneumonia or enlarged lymph nodes.
Common symptoms in children do include:
- Sore throat (sometimes seen in adults too).
- Diarrhea.
- Runny or stuffy nose.
Initially, it was not known that diarrhea could be a primary complaint of some COVID-19 patients. But a small study published in The American Journal of Gastroenterology found that digestive symptoms are common, occurring as the chief complaint in nearly half of patients.
The authors gathered data on 204 patients with COVID-19 in three hospitals in Hubei province.
The American Academy of Otolaryngology has proposed adding anosmia, or loss of the smell, to the list of screening tools for COVID-19 in the absence of other respiratory illnesses such as allergies.
On March 23, the WHO said they have a handle on major symptoms.
"A loss of smell or a loss of taste is something that we're looking into and we're looking forward to the results of the early investigations that are being conducted by a number of countries so that we have a more evidence-based approach and we can add that to the list," Maria Van Kerkhove, the head of WHO's emerging diseases unit, told reporters.
Not everyone will present with symptoms
Not everyone who is infected with COVID-19 has symptoms, and some people will only exhibit very minor symptoms.
"About 80 per cent of people will not get really sick from this," Dr. Samir Gupta, a respirologist, told CBC News.
And one of the more troubling discoveries about the illness is that an asymptomatic individual can transmit the virus to others. Contrary to what public health officials believed in the early weeks of the outbreak, a growing body of research indicates people don't have to appear ill at all to infect others.
The only way to confirm COVID-19 is with a lab test. Symptoms may appear as soon as two days after exposure or as long as 14 days after exposure.
The flu vaccine will not protect you against COVID-19.
What should you do if you have symptoms?
If you are under 50 years old and otherwise healthy, just stay home and take care of yourself. Definitely don't go to hospital, says Dr. Andrew Morris, an infectious disease specialist at Mount Sinai Hospital in Toronto.
"The hospital's like the worst place for anyone, other than people who are really sick and who will need hospitalization. Just being infected with a viral infection is not a reason to go to hospital."
But it is a good reason if you are older, have a compromised immune system, or are experiencing shortness of breath.

The most important thing to do is to call ahead to your health care-provider when possible, whether you are going to see your primary care physician, a walk-in clinic, or an emergency department at a hospital. Upon arrival, you will be asked to wear a mask while waiting to prevent spreading your germs and you may be isolated.
When you see the doctor, the Public Health Agency of Canada (PHAC) website stresses you should make sure to tell them:
- Your symptoms.
- Where you have been travelling and living.
- If you have had direct contact with animals (for example, visited a live animal market).
- If you have had close contact with a sick person, especially if they had fever, cough or difficulty breathing
As mentioned earlier, some people will be completely asymptomatic — and still come up positive.
"That's striking," Gupta said, "because the other 20 per cent will be quite sick. They'll need hospital, they'll need oxygen, and about five per cent of the total will be really sick and will be on a ventilator. "
Who is at greatest risk?
Canadians at greatest risk for developing more severe COVID-19 disease include those:
- Aged 65 and over.
- With compromised immune systems.
- With underlying medical conditions.
How is COVID-19 diagnosed?
Respiratory samples are processed by provincial labs. The labs may screen for other things first, such as the seasonal flu. The sample will only be sent to the National Microbiology Laboratory in Winnipeg should further testing be required.
What if I have COVID-19 but get sent home?
Public health officials recommend self-isolating: staying home and even keeping away from family members.
"The key is maintaining distance," Gupta said. "It means separate bedrooms, separate bathrooms, a minimum of six feet distance (about two metres), because that's how this spreads, through droplets which can travel up to six feet."
If you must leave home, PHAC says you should wear a mask or cover your nose and mouth with a tissue and maintain a distance of at least two metres from other people.
What if my child has symptoms?
To date, children do not seem to get very sick from COVID-19. Most healthy kids will get over it in a few days, as they would a common cold or the seasonal flu.
But if your child is sick, you should keep them home. With schools across Canada closed, that's a little easier now. Definitely keep them away from others, especially older family members or relatives.
"If you've got one kid who has coronavirus, chances are they're exposed to one to three older people who are at risk, who may end up in the hospital," said Morris.
One recent study found that the virus can still be detected in children long after they recover. While nasal swabs tested negative for the disease after two weeks, in some cases rectal swabs came back positive up to four weeks after hospital admission. However, scientists don't yet know whether the disease can be transmitted via feces.
How can you avoid infection?
There is no vaccine to prevent the infection, but health organizations, like PHAC here in Canada and the Centers for Disease Control in the U.S., recommend these preventive actions to help stop the spread of any respiratory viruses:
- Wash your hands often with soap and water for at least 20 seconds or use an alcohol-based hand sanitizer, with an alcohol content of at least 60 per cent.
- Avoid touching your eyes, nose, and mouth with unwashed hands.
- Avoid close contact with people who are sick, and stay home if you are sick.

Will a mask protect me from catching COVID-19?
After the SARS outbreak, PHAC asked a panel of medical experts for guidance on how flu is transmitted and how best to protect against infection, including the efficiency of face masks.
The report found that masks can offer protection, but there's no evidence inexpensive masks can protect against flu virus particles small enough to be inhaled into the lower respiratory tract or the lungs. It did find that the N95 masks are the most likely to be efficient, because they filter particles smaller than one micron and provide a tight facial seal.
Early on in the COVID-19 outbreak, Canada's chief public health officer, Dr. Theresa Tam, said that wearing a mask when you're well is not an effective measure for keeping yourself safe from infection.
But the science and advice has changed.
On April 6, Tam told reporters that wearing a non-medical mask can help stop the spread of COVID-19, in large part by protecting those around you. But she stressed the importance of doing so in tandem with other physical distancing measures and handwashing.
"A non-medical mask can reduce the chance of your respiratory droplets coming into contact with others or landing on surfaces," Tam said. "The science is not certain, but we need to do everything that we can, and it seems a sensible thing to do."
WATCH | Tam explains how wearing a non-medical mask can help reduce transmission:
Wearing a mask could give people a "false sense of security" that could encourage wearers to relax physical distancing, she also said.
"It can sometimes make it worse — if the person puts their finger in their eye or touches their face under their mask."
With files from Michelle Ghoussoub, Emily Chung, Brandie Weikle and The Canadian Press

